Psoriasis- one of the most common diseases, the frequency of which in the population is constantly increasing every year. And if we consider that absolutely all age categories are susceptible to this pathology, and its simple form quite quickly turns into a more complex form, then the question of proper therapy and prevention is really very acute. .
According to statistics, about 30 inhabitants of the planet suffer from this disease to one degree or another. What to do for those who contract psoriasis? What drugs and folk remedies can be treated? How to organize your meals well? Finally, let's put all the points.
Psoriasis and its causes
Psoriasis is an autoimmune disease with a rather vague etiology - the exact cause, despite many studies in this area, is still unknown. It is believed that this pathology is a consequence of genetically determined changes in the immune system, as a result of which chronic inflammation of the skin develops. However, its multifactorial nature is not excluded either - in other words, the involvement, with heredity, and the influence of the external environment.
It is worth noting that the predisposing factors, according to scientists, are quite different depending on the age groups: for example, whether various types of bacterial infections, including, in particular, strep infections, are considered to be triggers inchildren, then in adults stress stimuli and nicotine abuse are paramount, as well as alcohol, obesity and the use of certain drugs (eg, adrenaline receptor blockers).
It is impossible to completely cure psoriasis, however, modern medicine is quite capable of significantly alleviating the course of the disease and maintaining long-term remission in the patient.
There are several theories to explain the onset of psoriasis:
- infectious and parasitic;
- neurogenic;
- endocrine;
- metabolic;
- immunological;
- hereditary;
- theory of molecular mimicry.
As with many other conditions, the cause of the skin problems must be found in the intestine. Its length is 4-6 meters, and the inner surface is covered with villi, the total area of which is comparable to the size of a tennis court - this allows the absorption processes to proceed much more efficiently. Interestingly, the cells of the mucous membrane of the small intestine are completely renewed every 3-5 days. Here, moreover, up to 70% of human immunocytes are concentrated. So, one of the most common causes of psoriasis is considered to be leaky gut syndrome (LEPS).
Any deviation from the normal functioning of the intestinal mucosa leads to malabsorption, that is, a violation of the assimilation of basic nutrients (proteins, fats, carbohydrates, vitamins, minerals). In addition, the negative impact on the body of toxins and allergens increases: under such conditions it is much easier for them to get into the bloodstream. The direct link between psoriasis and inflammatory bowel disease has been proven in numerous studies.
Other scientific work confirms that a special microflora forms on the skin of a patient with psoriasis, which is significantly different from the microbiome of healthy skin.
In the area of psoriatic lesions, a mass of various bacteria is concentrated, the stability of which is significantly lower than that of normal skin - in particular, colonization with Staphylococcus aureus is observed, which has an extremely negative effect on theevolution of the inflammatory process.
Types of psoriasis
- Plaque psoriasis. . . In 90% of cases, dermatologists are faced with this particular form of the disease, also called simple or ordinary. First, small, separate areas appear on the skin, raised above the level of the healthy dermis. These inflamed areas are called psoriatic plaques. Gradually they grow, merging with neighboring places into a whole.
- Reverse psoriasis.This diagnosis is given to patients who develop smooth red spots in the folds of the skin and inside the folds - in the groin area, on the inside of the thighs, under the breast. Unlike simple psoriasis, the foci of inflammation are practically not covered with scales, but due to their location and constant friction, they cause severe discomfort to patients. In addition, there is a risk of reinfection with streptococcus or fungus, since in those places where the spots are localized, due to high humidity and temperature, ideal conditions are created for the reproduction of micro-organizations.
- Guttate psoriasis.This type of disease gets its name from the form of the formations. The lesions appear as a drop, raised above the level of healthy skin. A common trigger for this form of psoriasis is a previous strep infection, as we mentioned earlier. The fact is that the patient's immunity, affected in the fight against infection, is seriously weakened - his resources are not unlimited, and, like all living things, it takes time to recover - and thisis in this context that an autoimmune disease is activated.
- Pustular psoriasis.It is considered the most severe form, accompanied by the formation of blisters filled with a clear liquid. Inflammation of the skin begins around the foci, swelling and thickening appear. With a secondary exacerbation, the probability of which is quite high, the blisters fill with pus. Localized foci of pustular psoriasis on the arms and legs. In difficult cases, there is a ubiquitous localization of blisters on the body, their rapid growth and the risk of infection of the entire surface of the skin.
- Psoriasis on the nails.This type of disease changes the appearance and structure of the nail plates on the hands and feet. The nails thicken, lose their natural color, have an unpleasant smell. The skin around the nail bed becomes coarse, thick ridges are formed. In advanced cases, the nails may disappear without further regrowth.
- Psoriatic arthritis.In this case, the disease affects the joints and connective tissues. Most often, inflammation affects the distal phalanges of the extremities. There is psoriatic dactylitis - swelling of the fingers. The hip and knee joints are also at risk from the devastating effects of the ongoing disease. There are frequent cases of disability with loss of the ability to move independently.
- Psoriatic erythroderma.Scaly patches appear on the skin, while the peeling of the affected layer is observed. Patients experience extreme discomfort due to constant itching and swelling. Most often, this diagnosis is made in patients who have already been treated for simple psoriasis, but have not completed treatment or have changed medication.

Symptoms of the disease
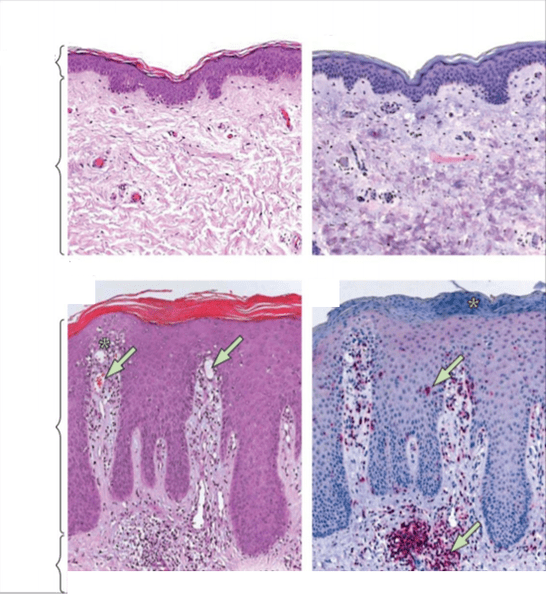
The first manifestation of psoriasis is a small rash on the skin. Papules grow rapidly, reaching spots with a diameter of 4-8 cm, they become more and more numerous, and dry scales form on the surface. In advanced cases, the individual spots merge with each other and the lesion affects large areas of the body. Psoriatic papules are distinguished from other skin diseases by their round shape with clear boundaries, bright red or pink color, and silvery white scales. They first appear on those areas of the skin, the integrity of which is violated as a result of abrasions, wounds, frostbite, constant rubbing. There are three characteristic signs confirming the onset of the development of psoriasis:
- Stearin stain phenomenon- dry particles easily separate from the affected surface, revealing an area that looks like a drop of wax or sterol.
- Psoriatic phenomenon(terminal) movie. Further cleansing the papules from the scales allows you to see a transparent and moist film, the skin under which is inflamed.
- Auspitz phenomenon. . . Removal of the terminal film leads to the appearance of the smallest drops of blood on the surface of the stain.
This psoriasis triad is unique - its presence undoubtedly allows for the correct diagnosis. Nevertheless, different parts of the body have their own characteristics of manifestation of the disease.
- Psoriasis on the body.The back, neck, abdomen, thighs, and lower legs are most commonly affected by guttate psoriasis. Small papules, which resemble drops in shape, gradually develop, rising above the surface of the skin. This form of the disease is often diagnosed in people who have had a staph infection.
- Psoriasis on the hands.The most common places for the appearance of psoriatic papules on the hands are the elbows and interdigital spaces - while, as a rule, a plaque form is observed, in which small individual fragments merge into a single area oflesion covered with dry scales. The forearms are much less likely to be affected.
- Psoriasis on the legs.The disease begins with single rashes in the knee area. Inflamed areas disturb patients with severe scaling and itching, rapidly increase in size and merge with neighboring areas.
- On the palms and feet.In most cases, the simultaneous defeat of the palms and feet is recorded, but in some patients the disease affects the stratum corneum of the purely upper or lower extremities. Due to the growth of psoriatic papules, thickening, enlargement of the skin occurs with further cracking.
- Scalp psoriasis.First of all, rashes appear on the forehead, back of the head and also behind the ears. First, patients note in themselves unique scaly formations that develop, merge with those located nearby, and over time can affect the entire scalp. The papules are very itchy, causing a constant urge to scratch the skin - the resulting sores and cracks are likely to become the gateway to infection. Dry particles are separated from damaging formations - first small, somewhat dandruff-like, then larger flakes.
- On the face, ears, neck.The localization of psoriatic papules on the face is rather an exception in the usual clinical picture. In rare cases, when this occurs, the disease affects the areas around the eyes and eyelids, as well as the cheeks and tongue. Formations on the neck quickly spread further - to the back or head. The ears are the site of the development of seborrheic psoriasis. Papules can appear both inside the cartilage shell and outside. When making a diagnosis, it is important not to confuse the disease with seborrheic eczema, which has similar symptoms.
- On the nails.There are three options for the initial manifestation of psoriasis on the nail plates. The first is the appearance of small pitted depressions. The second is thickening of the nails, a change in their natural color to gray or yellow. With the further development of psoriasis of the nails, the plaque exfoliates, the upper particles are easily separated. And, finally, the third is a deformation of the nail, accompanied by a loss of smoothness of the plate and the appearance of depressed areas.
- Symptoms of psoriasis in children.At an early age, the disease proceeds differently: the main localization of red, scaly rashes are skin folds: inguinal, in the elbow and popliteal folds, on the neck. Papules itch a lot, children experience constant torment, become irritable and restless. In general, all of the clinical variations seen in children are similar to those seen in adults. The differences concern only the manifestations, the localization of the pathological process and the course of the disease itself.



4 stages of psoriasis
Clinical dermatology, based on the differences in symptoms, the degree of skin damage and the duration, distinguishes three stages in the course of psoriasis. However, there is an opinion that the initial stage should be recognized as another full-fledged stage in the development of the disease.
- Initial stage.The first signs of psoriatic lesions are small rashes. The places of their appearance may be different and depend on the type of disease. Primary papules are no more than 3 mm, painted in a pale pink color, which after 3-4 days is replaced by a gray bloom - dead dermis particles are formed on the spot. This process is accompanied by itching and burning, and the general state of health worsens. Usually, plaque formation at the initial stage takes up to three weeks, and at this time a person has a chance to slow down the development of pathology.
- Progressive.At this stage, the disease affects large areas of the skin: for example, with normal psoriasis, plaques are formed, with other forms, characteristic papules. During the development of the disease, individual spots merge with each other, covered with gray scales. The symptom by which the progressive stage is determined is the Köbner phenomenon (isomorphic reaction). Any damage to the skin after a while is accompanied by the appearance of a rash of psoriasis in this place. Another confirmation that the disease is actively developing is the appearance of drops of blood, similar to dew, after the plaque is removed. The duration of this stage depends on the type of lesion. On average, it takes two weeks to two months.
- Stationary scene.During this period, a thick grayish-white or gray crust forms. The pink rims disappear. The skin becomes rough, dry particles are constantly exfoliated from it. The itching and burning sensation becomes less bothersome, but it doesn't go away completely either. New papules do not form. This step can be quite long.
- Regressive stage.The last stage in the development of the disease, during which there is a gradual reduction and resorption of plaques. The itching does not bother anymore. A clear sign of regression is the symptom of Voronov, when the papules are surrounded by white rings. The discoloration of the spots occurs from the center to the periphery, as a result of which bizarre patterns form on the skin. At the end of the regressive phase, only those areas of the skin that differ slightly from the shade of healthy areas are reminiscent of psoriasis. It is not necessary to speak of a complete cure in the case of psoriasis. The end of the regressive stage indicates that the disease cycle has ended, which can return at any time. In order for remission to be prolonged, one should pay attention to health: avoid provoking factors, follow a diet, be observed by a dermatologist.
Examination plan for psoriasis
- General clinical analysis of blood.
- Research on the content of vitamins D, B12, folic acid in the blood.
- Blood test for ALT (alanine aminotransferase), AST (aspartate aminotransferase), direct bilirubin, alkaline phosphatase, gamma-glutamyl transferase, cholesterol with a lipid profile, creatinine, glucose, insulin, total protein.
- Blood for rheumatoid factor, c-reactive protein, uric acid, ASLO.
- Ferritin, transferrin, serum iron are indicators of anemia (in particular, chronic diseases).
- Thyroid panel: TSH, T4 sv, TK sv.
- Co-program.
- KhMS according to Osipov.
- Ultrasound of abdominal organs.
Traditional treatments for psoriasis
Early therapy.
The sooner a person who discovers the first signs of skin damage to see a doctor, the more likely they are to take timely measures that will prevent the rapid development of the disease and its transition to a chronic form - and, therefore, significantly improvethe overall standard of living.

One of the most common drugs prescribed at the onset of the disease is salicylic ointment. It has an anti-inflammatory and antimicrobial effect, has a keratolytic effect, due to which the plaques are freed from keratinized particles. To reduce itching, mothball ointment is also used.
Therapy at a progressive stage.
At this stage, an integrated approach to treatment is necessary and only an experienced specialist can provide it. Treatment is aimed at relieving symptoms by ridding the body of toxins. To normalize metabolic processes, intramuscular injections of calcium gluconate are often prescribed. Sodium thiosulfate relieves inflammation and eliminates manifestations of intoxication.
To moisturize the inflamed skin, special emulsions and salicylic ointment are used. Means containing tar are contraindicated at a progressive stage: they act irritating and increase the suffering of the patient.

When the intensity of inflammation decreases, physiotherapy procedures can be connected. Patients with psoriasis receive ultraviolet irradiation, PUVA therapy, and paraffin applications. Corticosteroids and cytostatics are not used unnecessarily, these powerful drugs are needed only in difficult and advanced cases.
To reduce allergic manifestations, antihistamines are prescribed and sedatives are prescribed to reduce nervousness. Diuretics help reduce swelling in inflamed skin and flush toxins from the body.
Stationary therapy.
At this point, the inflammation subsides, the plaques become covered with a dry crust. Therefore, funds are needed to alleviate the discomfort associated with the appearance of scales. These are tar shampoos, oil-based emulsions.
In many patients, ultraviolet irradiation and PUVA technique have a good effect. If there is no improvement, doctors prescribe cytostatics.
Therapy at a regressive stage.
In the last period of the disease cycle, constant correction of treatment methods is required, depending on the current condition of the patient. Prevention replaces active therapeutic actions.
The patient is given recommendations to change his diet and lifestyle in general. In order to prevent the return of the skin lesion, it is necessary to avoid stressful situations that trigger the formation of psoriatic plaques.
As a rule, doctors give patients the following advice:
- reconsider his lifestyle: adjust your diet, get enough sleep, move more;
- ensure normal vitamin levelsD, iron, B vitamins, protein in the body;
- normalize the digestive tract: exclude hypoacidity, impaired flow of bile, SIBO and CIGR (syndromes of excessive bacterial growth and, therefore, fungal);
- get rid of foci of chronic infection: disinfect the oral cavity, undergo treatment with an ENT doctor;
- treat concomitant somatic pathology: hypothyroidism, insulin resistance, metabolic syndrome, etc.
Traditional methods to get rid of psoriasis
- Initial stage.At the first sign of skin damage, juniper and lavender oils are effective. They soothe irritated areas of the dermis, promote healing of minor injuries, relieve the feeling of tightness. A few drops of oil are added to a cream of neutral composition, for example, for children, and applied to the rash that appears. Another popular method of treating the initial manifestations of psoriasis is the use of 3% hydrogen peroxide. All measures, even the most harmless at first glance, can be applied after consulting a dermatologist. Diet changes, avoiding unhealthy foods, and alcohol are also common recommendations from traditional healers.
- Progressive stage. At the stage of rapid development of the disease, an infusion of celandine is added to healing oils and hydrogen peroxide. To prepare it you will need fresh or dried plant stems and salt water. Alcoholic tinctures are contraindicated, they can worsen the condition of the affected skin. It is necessary to insist on celandine for at least several hours, and before applying the healing solution to the plaques, treat them with birch tar.
- Stationary scene.At the stage of the end of the formation of new papules, you can use proven folk methods, which certainly will not harm the patient. These include the use of sulfuric ointment, salicylic solution.
- Regressive stage.At the final stage of the course of the disease, hirudotherapy (leech therapy) is often used. Although this method is not officially recognized by traditional medicine, many experts do not exclude its effectiveness. The procedures are carried out within 3-10 days, depending on the patient's state of health.

Prevention of psoriasis: how to prevent the development of the disease
- Skin care.To minimize the risk of psoriatic lesions in the presence of a genetic predisposition, simple ways to maintain skin health will help: water and hardening procedures (swimming in the sea, baths with herbal extracts and salts, showerscontrast, sprinkling fresh water into the air, etc. ); use soft sponges and avoid hard washcloths which can damage the skin; the use of detergents, of natural composition, without aggressive chemical components.
- Ultraviolet rays.Several studies have proven the beneficial effect of sun exposure on skin prone to psoriatic plaque formation. Moderate doses of ultraviolet light help speed up tissue regeneration and reduce inflammation. Sunbathing should not be abused: too much rays can exacerbate the disease.
- Clothing.Synthetic fabrics, fitted styles, an abundance of belts and zippers - all this is contraindicated for patients with psoriasis, even in remission. Clothing must be natural, hypoallergenic, loose, not causing any inconvenience that could lead to the return of pronounced symptoms. Dark tones should be avoided for aesthetic reasons; silvery white scales are less noticeable on light colored clothing.
- Injuries.For patients with psoriasis, any small wound, scratch, abrasion can cause the return of the progressive stage and secondary infection of the skin. They must be extremely careful to avoid injury.
- Cosmetics and household products.Not all remedies are suitable for maintaining the cleanliness of people with such diagnoses. When choosing shower gels, soaps, shampoos, it is important to pay attention to their composition, favoring those that contain natural ingredients. It is better to buy therapeutic series of care products sold in pharmacies. Scrubs with solid particles are absolutely contraindicated: they are able to start the disease process again due to the smallest wounds on the skin. Household chemicals should also be selected based on health safety, do not use aggressive cleaning powders based on chlorine and alkalis. Gloves should be worn when cleaning to avoid negative effects on the skin of the hands.
- Vitamin therapy.Maintaining vitamin balance is indicated for everyone, and especially for people with chronic dermatitis. Complex preparations keep the body in good condition, help it resist viruses and prevent metabolic disorders.

Psoriasis- this is not a death sentence, but a very serious reason to reconsider the rules you used to live by. Your allies on the road to taming the disease should be competent professionals - dermatologists, nutritionists, therapists. With their help, as well as through a deliberate approach to treatment, you can learn to live comfortably, despite your diagnosis.























